The importance of cancer screening and closing the “COVID-induced screening gap”

Approximately 9.4 million cancer screening tests in the U.S. in 2020 were missed, largely due to the coronavirus pandemic.1 This “COVID-induced screening gap” gives rise to dire consequences, including death.2 A modelling study from the National Cancer Institute suggests there will be over 4,000 excess deaths from colorectal cancer alone from 2020 – 2030 due to the pandemic.3 Because of the vast impact of COVID-19 on cancer screenings, interventions have been implemented to reduce the gap, but there is more work to be done to maximize the rate of screening.
In this post, we will discuss the basics of cancer screening, with a focus on general population screening, and work that has been implemented to improve screening rates.
What is cancer screening?
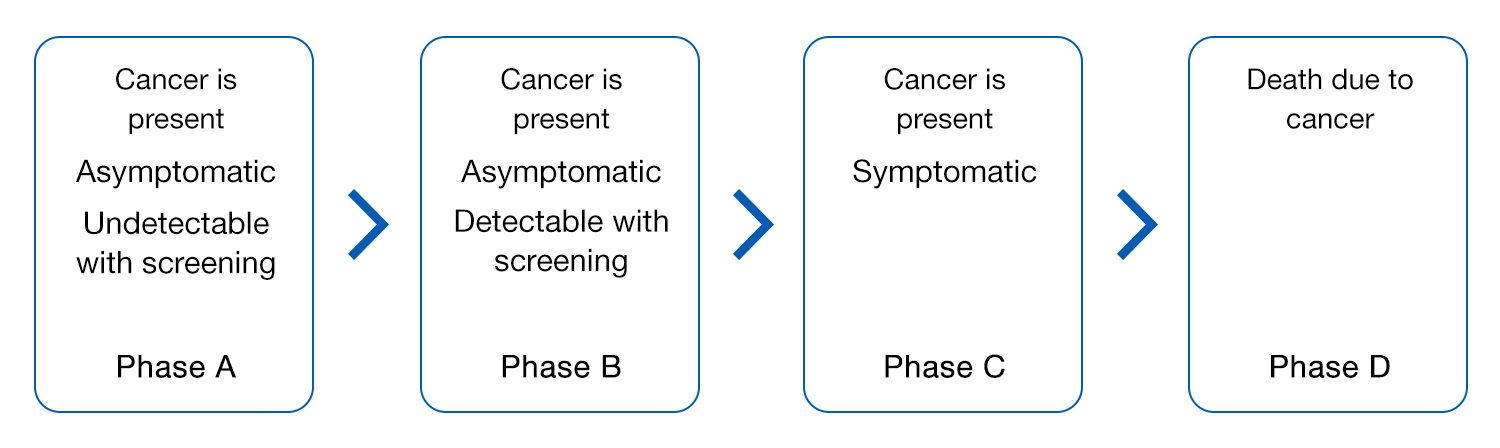
Cancer screening is a form of preventive care. An important goal of cancer screening is to detect cancer at an early stage before symptoms appear.4 In the figure below, phase B represents the point in time where screening can detect cancer.
Why undergo cancer screening?
As with most medical services, screening tests have both risks and benefits. For some cancers, including colorectal, breast, cervical, and lung cancer, the United States Preventive Services Task Force (USPSTF) has assessed that the benefits outweigh the harms in select groups.5
The advantage of detecting a cancer early is that, generally, the earlier a cancer is caught, the better the treatment response or curative rate. For some cancers, screening can also decrease the risk of dying from the cancer.4
Who should undergo cancer screening, and when?
Not all cancers have screening tests available or are recommended for routine screening. For those without an increased risk of cancer, major guidelines generally support screening for colorectal, breast, cervical, and prostate cancers. Lung cancer screening is recommended for certain individuals at an increased risk of lung cancer.
For each cancer, there are different populations that are advised to screen. For instance, the USPSTF recommends adults aged 45-75 without symptoms and who are at average-risk for colorectal cancer (CRC), to screen for CRC, while those aged 76-85 should have a discussion with their provider to determine if CRC screening is appropriate. “Average-risk” is defined as those without a prior diagnosis of colorectal cancer, adenomatous polyps, or inflammatory bowel disease and those without a personal or family history of certain genetic disorders that may put them at a higher risk of CRC.6

Efforts to reduce the gap in cancer screenings
When the pandemic struck, screenings declined. A few reasons for this decline include fear of going into healthcare institutions and institutions delaying non-emergency services. But now, many institutions are again offering these services, and there are multiple efforts to improve screening rates, particularly after the dip during the pandemic.1
One example is the Return-to-Screening study, a quality improvement project across hundreds of cancer programs that aimed to improve screening rates using interventions that have been proven to improve rates.7
Multiple institutions have also utilized noninvasive options to reduce the gap. For instance, colorectal cancer screening can be completed by a variety of noninvasive options. A study conducted at UCLA Health found that screening rates improved to even pre-pandemic rates after increased usage of noninvasive screening methods.8
To reiterate, cancer screenings are intended to be used in individuals without symptoms. However, as mentioned in our previous blog article here, a survey revealed an interesting statistic: 1/3 of participants said their primary reason for not getting screened was that they were asymptomatic. It is important to remember that cancer screening is a form of preventive care which allows for earlier detection of cancer and ultimately, potentially better treatment (or even a cure!).
Additional Information
This blog does not provide medical advice. If you would like more information on cancer screening, please reach out to your primary care provider to discuss the benefits and risks. You can also find more information here from the American Cancer Society.9